Brexpiprazole: A New Frontier in Mental Health Treatment
Brexpiprazole, marketed under the brand name Rexulti, is a medication classified as an atypical antipsychotic. Atypical antipsychotics differ from older antipsychotics, known as typical antipsychotics, in their ability to target specific neurotransmitter systems in the brain, resulting in reduced side effects. Brexpiprazole is primarily used to treat schizophrenia and major depressive disorder (MDD), but it also has several other potential applications.
Pharmacology of Brexpiprazole
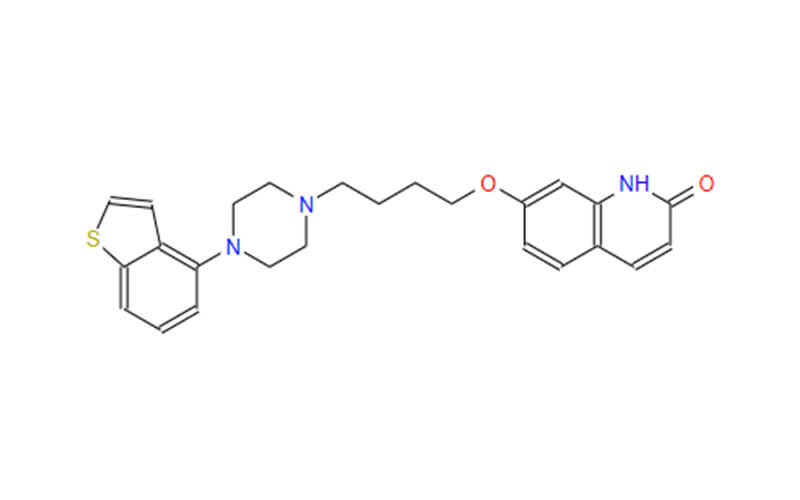
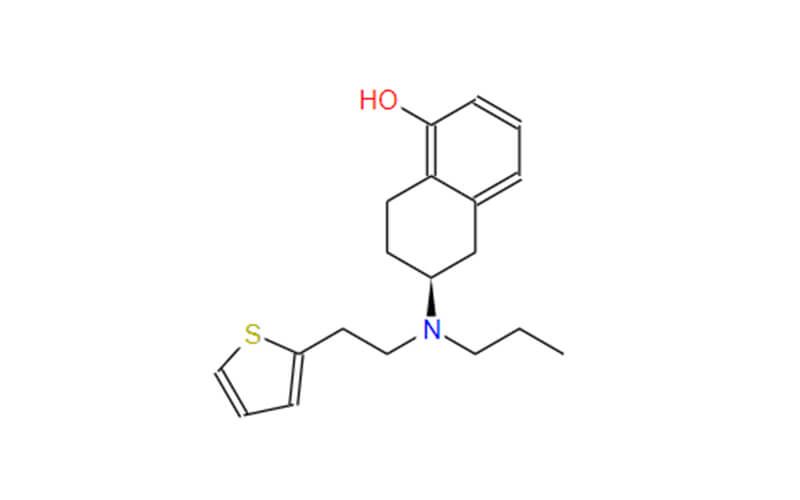
Brexpiprazole’s mechanism of action involves modulating the activity of dopamine and serotonin receptors in the brain. Dopamine and serotonin are neurotransmitters that play crucial roles in regulating mood, cognition, and behavior. Brexpiprazole acts as a partial agonist at serotonin 5-HT1A and dopamine D2 receptors, meaning it has the ability to both activate and block these receptors. Additionally, it acts as an antagonist at serotonin 5-HT2A receptors, blocking their signaling activity. This complex interplay of receptor interactions is thought to contribute to Brexpiprazole’s therapeutic effects.
Following oral administration, Brexpiprazole is rapidly absorbed into the bloodstream, reaching peak concentrations within 2 to 3 hours. It is extensively metabolized in the liver and eliminated through the feces and urine. The elimination half-life of Brexpiprazole is approximately 24 hours, indicating that it remains active in the body for a day after a single dose.

Therapeutic Uses of Brexpiprazole
Brexpiprazole is approved for the treatment of various psychiatric conditions, including:
- Schizophrenia: Brexpiprazole effectively controls the positive and negative symptoms of schizophrenia, such as hallucinations, delusions, disorganized thinking, and social withdrawal.
- Major Depressive Disorder (MDD): Brexpiprazole is used as an adjunct therapy to antidepressants in patients with MDD who do not adequately respond to antidepressant treatment alone.
- Schizoaffective Disorder: Brexpiprazole effectively manages the mixed symptoms of schizophrenia and depression seen in schizoaffective disorder.
In addition to its primary indications, Brexpiprazole is also being investigated for potential use in other psychiatric conditions, such as bipolar disorder, obsessive-compulsive disorder, and Tourette’s syndrome. Early research suggests that Brexpiprazole may be effective in these disorders, but further studies are needed to confirm its safety and efficacy.
Brexpiprazole Side Effects
Brexpiprazole is generally well-tolerated, but it can cause a range of side effects. The most common side effects are mild and transient, including headache, constipation, diarrhea, and weight gain. These side effects are typically manageable and often resolve on their own.
More serious side effects can occur, although they are less common. These include tardive dyskinesia, a movement disorder characterized by involuntary muscle movements, hyperglycemia (elevated blood sugar levels), and neuroleptic malignant syndrome (NMS), a rare but potentially fatal condition characterized by muscle rigidity, fever, and altered mental state.
Comparison of Brexpiprazole with Other Atypical Antipsychotics
Brexpiprazole shares some similarities with other atypical antipsychotics in its ability to effectively treat schizophrenia, MDD, and schizoaffective disorder. However, it also possesses unique characteristics that set it apart from its counterparts.
Similarities
- All atypical antipsychotics act primarily on dopamine receptors, with varying degrees of affinity for different receptor subtypes.
- All atypical antipsychotics are generally effective in treating the positive and negative symptoms of schizophrenia.
Differences
- Brexpiprazole’s dual action on serotonin and dopamine receptors may contribute to its lower risk of extrapyramidal side effects (movement disorders) compared to some other atypical antipsychotics.
- Brexpiprazole’s favorable side effect profile makes it a suitable choice for patients with treatment-resistant depression or those with a history of adverse reactions to other antipsychotics.
Despite these potential advantages, Brexpiprazole may not be the best choice for all patients. The decision of which atypical antipsychotic to use should be made on a case-by-case basis, taking into account individual patient factors and preferences.

Conclusion
Brexpiprazole has emerged as a valuable addition to the armamentarium of antipsychotic medications. Its dual action on serotonin and dopamine receptors, combined with its favorable side effect profile, makes it a promising option for treating a range of psychiatric disorders, including schizophrenia, major depressive disorder, and schizoaffective disorder. While close monitoring by a healthcare professional is essential, Brexpiprazole offers a safe and effective treatment option for many patients seeking relief from these debilitating conditions.